A predictable patient revenue layer
for RCM organizations.
RCM organizations are being asked to do more than ever — not just manage insurance reimbursement, but also improve patient billing outcomes.
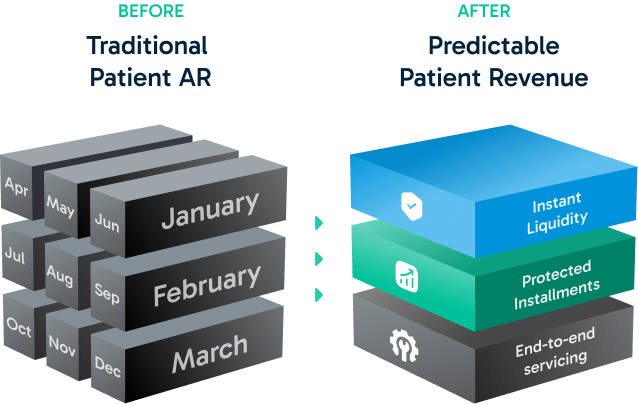
As patient responsibility grows, traditional billing and in-house payment plans introduce operational strain, missed payments, and AR volatility.
Credee strengthens the RCM offering by embedding a revenue layer that improves patient collections without increasing operational workload.
AR grows.
Cash doesn’t.
Even when billing and collections are well-run, patient responsibility, failed payments, and long in-house plans push revenue further into AR — while realized cash becomes slower and less predictable.
Credee adds a missing layer to the RCM model: revenue predictability and optional liquidity, embedded directly into patient billing workflows.
More collected revenue = More fees earned.
Credee increases what ultimately gets collected by:
Enabling full or partial acceleration
on future receivables.
Reducing long-term
write-offs
Protecting a portion of payment plan
revenue from missed payments
When providers collect more — RCM earns more.
This is not a pricing change. It’s a revenue expansion.
Expand your capabilities. Not your team.
Instead of building billing operations, patient outreach, and exception handling in-house, Credee serves as an embedded infrastructure layer that manages servicing, follow-ups, and compliance end-to-end — reducing labor burden while improving payment completion and predictability.
Pre and post-service revenue capture.
Credee supports revenue capture before and after service, without disrupting existing workflows.
Pre-Service
Out-of-pocket estimates enrolled into payment plans
Flexibility improves patient commitment
Plans can be adjusted post-adjudication
Post-Service
Invoices and statements include payment plan options
Patients opt in through familiar portals
Revenue protection and acceleration become available to providers
